By Wendy Lee Nentwig
By now we all know the drill: Wash your hands, wear a mask, keep your distance, stay home. Has our country ever been more health-conscious? The COVID-19 pandemic has forced us to focus on our physical health in order to avoid getting sick or passing on the virus unsuspectingly. But now health experts are warning about a new crisis heading our way.
“As many as 75,000 Americans could die because of drug or alcohol misuse and suicide as a result of the coronavirus pandemic.”
“The coronavirus pandemic is pushing America into a mental health crisis,” The Washington Post blared in a May 4, 2020 headline. “As many as 75,000 Americans could die because of drug or alcohol misuse and suicide as a result of the coronavirus pandemic,” CNN added, citing analysis conducted by Well Being Trust, a national public health group.
We’ve been so busy washing our hands and worrying about losing our jobs, that we haven’t taken the time to consider the mental toll the coronavirus is taking. “Anxiety and depression are rising,” according to The Washington Post, “and the US is ill-prepared.”
Coronavirus’ Mental Health Fallout
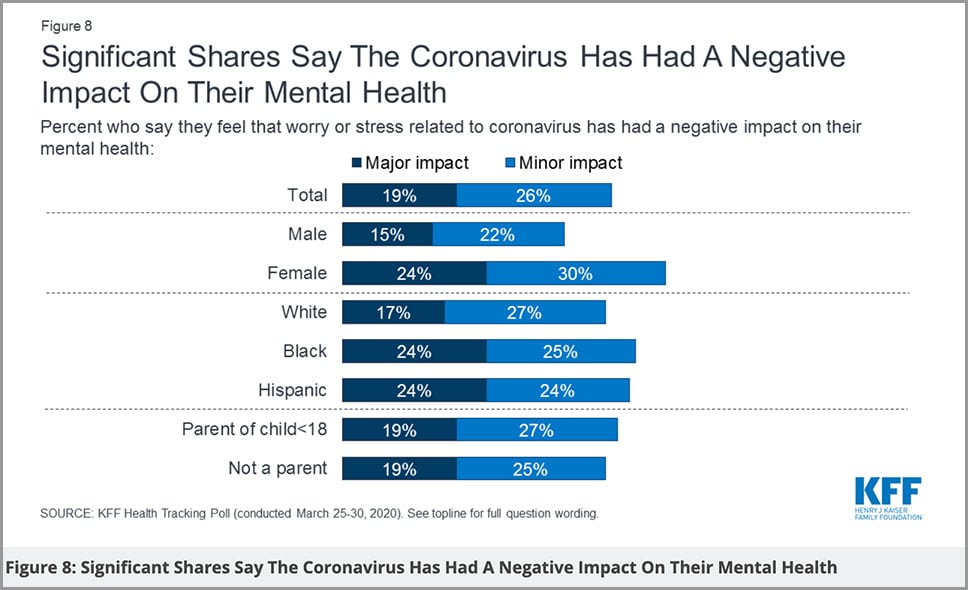
The growing unemployment crisis, economic downturn, and stress caused by isolation and lack of a definitive end-date for the pandemic are taking their toll on many of us. Nearly half of Americans report the coronavirus crisis is harming their mental health, according to a Kaiser Family Foundation poll.
A federal emergency hotline for people in emotional distress registered a more than 1,000 percent increase in April compared with the same time last year. Roughly 20,000 people texted that hotline, run by the Substance Abuse and Mental Health Services Administration in April 2020, according to The Washington Post. “Online therapy company Talkspace also reported a 65 percent jump in clients since mid-February. Text messages and transcribed therapy sessions collected anonymously by the company show coronavirus-related anxiety dominating patients’ concerns,” The Post also reported.
The suicides of two New York healthcare workers also highlight the growing problem, but out of the trillions of dollars Congress passed in emergency coronavirus funding, only a small fraction is allocated for mental health.
Mental Health In the Spotlight
“A federal emergency hotline for people in emotional distress registered a more than 1,000 percent increase in April compared with the same time last year.”
From an early age we were taught the importance of regular check-ups, annual physicals, and the need for trips to the doctor when not feeling well. We use a thermometer to screen for fevers, but how do we take our mental temperature?
According to the National Council on Behavioral Health, 76% of Americans think mental health is just as important as physical health, but wellness checks rarely include questions about how we’re doing mentally. We stay home and rest when we have the flu, but 52% of Americans have tried to “grin and bear it” instead of seeing a doctor when feeling depressed or mentally unstable, according to America’s Mental Health Campaign. Often, they don’t know where to turn.
May is also Mental Health Awareness Month. First observed in the US in 1949, it was started by Mental Health America to bring attention to mental health issues. We’ve come a long way in understanding that we need to take care of ourselves physically, emotionally, and mentally, but more than 70 years after that first Mental Health Month, we still have far to go. Just look at these staggering figures:
- Those with mental illnesses tend to have higher mortality rates than those without them. (Source: World Health Organization)
- Suicide claims more than 800,000 lives annually worldwide. (Source: World Health Organization)
- Approximately 15 percent of the world’s diseases are mental illnesses. (Source: National Alliance On Mental Illness)
- In the United States, an estimated one in five adults —44 million people — experience mental illness each year. (Source: National Alliance On Mental Illness)
Mental health issues can also make someone at a higher risk for addiction, eating disorders, or other co-occurring conditions. Physically or emotionally traumatized people are at much higher risk for drug use and substance use disorders, according to the National Institute on Drug Abuse (NIDA).
A Proactive Response
The predictions for a COVID-related mental health crisis may be grim, but there are actions we can take to change those projected numbers. That’s why Well Being Trust and other mental health professionals are sounding the alarm now, in hopes that local, state, and federal authorities will take action before we have a new crisis on our hands.
Meadows Behavioral Healthcare has been responding to the global pandemic in a variety of unique, proactive ways to help people cope. Rio Retreat introduced a new Surviving Social Distancing online workshop. This timely 4-day intensive allows participants to take a look inside themselves and turn this time of increased anxiety and isolation into an opportunity for personal growth. There’s also a 1-day version scheduled for May 18.
Meanwhile, MBH’s Chief Medical Officer, Dr. Jon Caldwell, penned an article titled Leaning Into Fear, which explores three of our most common fears and how leaning in can help loosen fear’s hold on us. He also participated in a Facebook Live event with the same title, discussing fear during the time of COVID-19.
Our Senior Fellows have also been offering COVID-related insight and advice. Dr. Tian Dayton’s COVID-19: When Hidden Grief Is Triggered looks at how we can address underlying issues that surface during this time. Then over on The Meadows Ranch blog, Jenni Schaefer’s post, Recovery From Six Feet Away: Connection, Creativity, Coronavirus, explores how those in recovery for eating disorders can stay connected to their support systems while social distancing.
Time to Act
“Just as the country took drastic steps to prevent hospitals from being overwhelmed by infections, experts say, it needs to brace for the coming wave of behavioral health needs,”
We can turn the tide, but we need to act fast. Meadows Mental Health Policy Institute, a Texas-based nonprofit not affiliated with Meadows Behavioral Healthcare, created models that suggest if unemployment amid the coronavirus pandemic ends up rising five percentage points to a level similar to the Great Recession, an additional 4,000 people could die from suicide and an additional 4,800 from drug overdoses. But if unemployment rises by 20 percentage points — to levels recorded during the 1930s Great Depression — suicides could increase by 18,000 and overdose deaths by more than 22,000, according to Meadows.
“Just as the country took drastic steps to prevent hospitals from being overwhelmed by infections, experts say, it needs to brace for the coming wave of behavioral health needs,” The Post article insists. We all need to do our part by looking out for each other and taking stock of how we’re doing mentally during this crisis. If you need help, seek it. Treatment is available to address trauma, depression, and other co-occurring issues —whether they’re related to COVID-19 or this time of isolation has simply brought them into focus.
“We can change the numbers — the deaths have not happened yet,” Well Being Trust’s chief strategy officer Dr. Benjamin F. Miller told CNN. “However, it is on us to take action now.”

